What is quality improvement in healthcare?
Quality improvement (QI) is the ongoing process of systematically targeting improvement in specific aspects of healthcare. Healthcare organisations that engage in quality improvement typically utilise a particular QI model such as Six Sigma, Plan-Do-Study-Act, or Lean. Quality improvement is not a single activity, but rather a series of operations intended to positively impact patient care.
Quality improvement requires a continual commitment to making data-driven process improvements to increase the quality of care within a healthcare system.
Discover how Qualtrics Patient XM drives Quality improvement
Why quality improvement?
The main goals of quality improvement in healthcare are to positively impact clinical outcomes and patient satisfaction, and reduce healthcare costs. In recent years, the Centers for Medicare and Medicaid Services (CMS) has begun to mandate participation in quality improvement initiatives as part of many regulatory and value-based reimbursement programs.
Only 45% of patients believe the quality of their healthcare has been good or very good. The relation between quality of care, patient outcomes, and healthcare costs calls for a more calculated approach to quality measurement and improvement.
The good news is that technology has provided a way for healthcare systems to collect and measure the data needed for enhancing organisational performance and in turn, improving health care quality.
What is the impact of quality improvement in healthcare?
Quality improvement takes planning and dedication, but the payoff is significant.
According to the 2021 National Healthcare Quality and Disparities Report published by the Agency for Healthcare Research and Quality (AHRQ), quality improvement directly correlates to better patient outcomes and reduced healthcare costs. Improved quality in areas such as person-centred care, care coordination, patient safety, affordable care, effective treatment, and preventive care contribute to:
- Improved health status and outcomes
- Reduced risk of mortality
- Reduced readmissions
- Reduced harm and hospital-acquired conditions
- Reduced healthcare costs
Let’s take a closer look at some of the rewards of healthcare quality improvement initiatives.
The impact of quality improvement on patients
One major focus of healthcare quality improvement is to improve patient care. Quality improvement has been proven to have a positive impact on patients.
Improved clinical outcomes
Quality improvement results in better patient outcomes. QI initiatives can be used to improve treatment and medication adherence, as well as patient comprehension. Healthcare professionals can also use quality improvement to foster stronger relationships with patients, which has been proven to lead to greater health outcomes.
Patient access barriers can also be addressed with quality improvement. Focusing QI projects on scheduling and other factors affecting timely access to care improves the ability for more patients to receive treatment, and with less delay.
Reduced readmissions
Higher hospital readmission rates are associated with lower patient experience scores. An average of 27% of readmissions are thought to be avoidable, prolonging patient recovery and increasing patients’ cost of care.
Quality improvement projects are essential to reducing preventable readmissions. Many health systems (like this one) have successfully lowered their readmission rates with quality improvement.
Enhanced patient experience
The patient experience is linked to health outcomes and patient loyalty. A wide variety of factors affects the patient experience and quality improvement is being used increasingly to help improve pain points during the care experience like communication, wait times, discharge, billing, and more.
The impact of quality improvement on costs and profit
There are many ways in which quality improvement efforts help organisations reduce healthcare costs, including:
- Reduced waste
- Reduced overuse of care
- Reduced hospital-acquired conditions
- Reduced hospital readmissions
- More cost-effective treatment
- Improved communication between patients and providers
Reduce readmission costs
Reduced readmissions don’t only benefit patients; hospitals and payers benefit, too. The average hospital readmission cost is over $15,000, and in 2021 nearly half of all hospitals faced financial penalties for high readmission rates. Quality improvement initiatives to identify and address the factors contributing to preventable readmissions can greatly impact these associated healthcare costs.
Get reimbursed through regulatory programs
Many healthcare entities are required to participate in federally regulated value-based care programs as well as incentive programs at the individual state level. Health care providers and systems are reimbursed based on fulfilling certain quality improvement measures. Through these programs, quality improvement is tied directly to financial rewards.
How do you measure quality improvement?
Quality improvement is a systematic process that involves identifying targeted improvement areas and then collecting data to standardise processes and achieve predictable outcomes. There are many components of a typical QI project:
- Identifying and prioritising target areas of improvement
- Designating an improvement team
- Establishing a baseline
- Collecting data
- Analysing and interpreting the data
- Implementing interventions
- Engaging in ongoing evaluation
What needs to be improved?
There are different ways you may come to determine improvement is needed in one or more areas of your health system. You may need to fulfil the requirements of a value-based care or incentive program. Alternatively, you may notice a trend based on observations such as increased patient no-shows, more readmissions for a certain patient population, or decreased productivity among administrative staff.
You’ll want to assign a quality measure for each area you’ve targeted for improvement. Measures help to clearly define the goal you’re hoping to achieve. Examples of quality improvement measures include:
- Reduce the amount of time a patient with a referral waits for an appointment
- Reduce the number of appointments for which patients do not show
- Increase patient-reported satisfaction with a certain type of treatment
- Increase patient willingness to recommend their provider
- Reduce nurse turnover within a unit
- Reduce the percentage of surgery patients with surgical complications or postoperative infection
You may also choose to utilise quality measures established and verified by The National Quality Forum, AHRQ, the Quality Payment Program, or the Institute for Healthcare Improvement.
Who is responsible for quality improvement?
Quality improvement should engage all the relevant players who will work together to achieve the best results. Research shows that there is better progress in the QI process when both clinical and non-clinical staff are engaged. In order to be successful, this improvement team should be engaged throughout the life of the QI project.
What type of data should you collect?
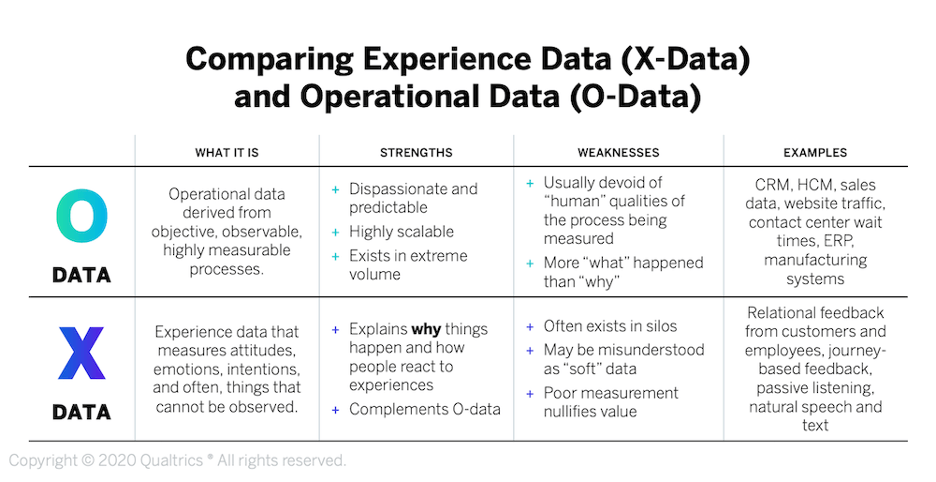
Quality improvement efforts rely strongly on data collection. To drive improvement, you’ll need to collect both operational data (O-data) and experience data (X-data). Operational data will help you to measure and track your efforts while experience data provides context surrounding your patients’ experiences.
Some of the data needed for quality improvement may come from EHRs, clinical data, or administrative data, but you may need to collect additional data for action planning and performance measurement.
Patient surveys
Patient surveys are a great tool for collecting data for quality improvement. Here are some best practices for using patient surveys to gather data in your quality improvement initiatives.
Survey best practice #1: Ask the right questions
The data you collect from patient surveys should help you to better understand the drivers of the outcome you hope to achieve. For example, if your goal is to improve patient satisfaction with the scheduling process, you may want to ask the patient how they scheduled that particular visit and offer a free-text option for the patient to share comments about their scheduling experience.
Survey best practice #2: Collect responses in real-time
Quality improvement is nearly impossible without timely feedback. Many healthcare organisations still rely on regulatory paper surveys for patient feedback; the delayed reporting methods for these surveys makes it very difficult to drive meaningful action from the results. A platform that delivers survey response data in real-time is essential to healthcare improvement.
Survey best practice #3: Reach out through all channels
These days, patients prefer to interact with their healthcare providers through a variety of channels. Ask patients for their feedback where they normally connect with you–by email, text, through your patient portal, etc.
Conversational data
With the right tools, even your communications with patients can be utilised for quality improvement. Conversational analytics provide insights into patient emotion, intent, and effort that would otherwise go undetected with traditional patient feedback collection.
The information gathered from conversational data can be valuable in action planning, change implementation, and improvement measurement.
What do you do with the data?
You’ve been collecting data with a quality improvement goal in mind. Now what? Here are three steps for assessing your improvement efforts.
Leverage data analytics
Analytics are the backbone of the quality improvement process. You’ll benefit the most from a platform with built-in analytics tools, dashboards, and visualisations to help you easily discover patterns, identify correlations, and monitor progress over time.
Data analytics help you to gauge the effectiveness of your improvement efforts. They also provide the insights needed to adjust components of health care delivery within your organisation.
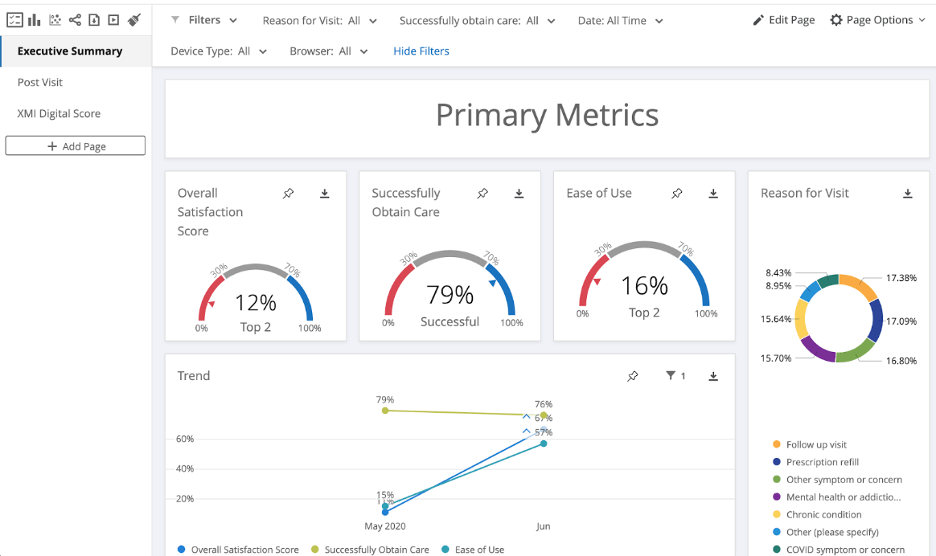
Each individual involved in the quality improvement process should have access to these analytics. Certain stakeholders may benefit from tailored visualisations and dashboards containing the information most relevant to their role in the improvement process.
Perform continuous monitoring
You’ll want to monitor your data continuously throughout the quality improvement process. Reviewing your data regularly enables you to:
- Understand what about your improvement approach is and isn’t working
- Make adjustments to steer you closer to your improvement goals
- Identify additional data needs
- Provide feedback to the improvement team and maintain a shared awareness of your progress
Drive quality improvement in healthcare with Qualtrics
Quality improvement is a complex process, but it’s made easier when you have the right tools at your fingertips. The Qualtrics XM for Healthcare solution is designed to collect and analyse your patient experience data all in one platform. Dashboards, visualisations, in-depth analytics, and EMR system integrations all work together to amplify your quality improvement efforts.
Discover how Qualtrics Patient XM drives Quality improvement